Veteran Finds Relief: Cube Conquers Night Sweats and PTSD
Chilipad Editorial Team • Sep 11, 2022

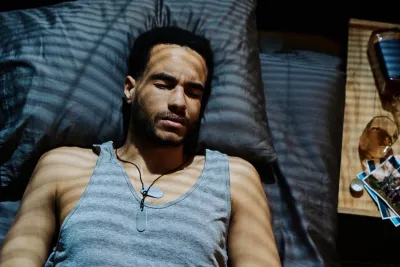
Recently we had the opportunity, and great honor, to chat with Dave, a 40-year-old Army veteran who had been experiencing sleep struggles after his separation from the military.
Dave spent the last 10 years of his career in Army Special Operations. He joined the Army after college in the early 2000s and deployed five times in support of named operations as well as countless unnamed ones.
Dave was dealing with a lot of sleep struggles, but like many people, didn’t know which products or tools could help.
Read More: Night Sweats in Men
Decrease the Severity of PTSD
Our cooling mattress pads can help reduce symptoms of PTDS. Take control of your body temperature, fall asleep faster, and wake up refreshed.
Sleeping Hot and Sleep Anxiety
Dave actually got connected with sleepme through a fitness coach at his local gym. The coach he met at the gym also works here at sleepme!
Through their conversations, she asked Dave if he’d like to be part of our company’s philanthropic mission with Sleepme Cares. This includes donating our innovative sleepme systems to veterans looking to improve their health and wellness.
Was he interested in trying it out? The answer was a resounding YES, and the rest, as they say, is history. It’s safe to say that Dave is now a very happy sleepme sleeper!
Read on to learn how the Cube, the original mattress cooling pad for your bed, helped Dave improve his sleep and, ultimately, reclaim his health and vitality!
I Was Scared to Go to Sleep...
Dave
40-year-old Army Veteran
Question:
On a scale of 1-10, with 10 being amazing, how would you have rated your sleep quality before using the Cube?
Answer:
I would rate it a 4. That is, I "slept"...closed my eyes, stayed reasonably still in a subconscious state for varying periods of time, but woke up generally feeling tired, sweating, irritable, and had many problems with migraine headaches.
Question:
Do you mind sharing more details about your sleep struggles?
Answer:
I wasn't sleeping well at all. I'd often wake up sweating to death, having to change clothes in the middle of the night, having trouble getting back to sleep because the mattress was wet with sweat. One night in particular, my fiancé took a video of me sleeping. I was snoring, and then I stopped breathing...for a minute and a half. I had no idea.
Question:
Which treatments did you try and were any effective?
Answer:
All three, and I'll address them collectively. Most people don't "wind-down" when they go to sleep. The lights are still on, they're still using devices with bright blue lights, and that tricks the brain into staying awake longer. I found that once I knew that I was snoring and having episodes of not breathing for periods of time, that I was scared to go to sleep and had severe anxiety about sleeping, especially before the actual sleep study which confirmed obstructive sleep apnea, one of the most common sleep disorders.
I also experienced sleep paralysis, where you wake up, your eyes are open, you are aware of your surroundings, but your body and muscles don't move. You are stuck in the position in which you slept for an indeterminable amount of time before your body "wakes up" along with your mind. I wear a CPAP every night now, which forces air into my nose so that my airways constantly stay open.
Question:
Did you try any other “lifestyle” strategies to improve your sleep?
Answer:
I've worked out and exercised for the last three decades, but never experienced any real progress in those goals until I was treated for sleep apnea and started losing weight with "diet" modifications as well.
Full disclosure, I don't "diet" in the traditional sense. I eat prescribed amounts of macronutrients (protein, carbohydrates, fats) daily depending on whether or not I'm working out that day, and in the last six months, I've dropped 30+ pounds as a result. If it fits within my numbers, I eat it. It doesn't matter what it is, within reason. But, if you eat junk, those numbers add up quickly and you'll end up not reaching your goals as quickly as a result.
I haven't tried meditation, but I generally try to stay positive, even when it's hard for me, and breathe when I'm stressed FIRST before saying or doing anything.
Question:
How was the overall Cube setup/install process?
Answer:
Pretty easy! The directions are easy to follow, fortunately I keep distilled water handy with the CPAP because you'll need that as well as some AAA batteries for the remote, but everything is fairly simple!
Question:
On a scale of 1-10, with 10 being amazing, how would you rate your sleep quality after using the Cube?
Answer:
I would rate it a 10! I fall asleep easier and my temperature is regulated! I'm still experimenting with the 'best' temperature setting. You know, what the CPAP does for my airways, sleep stages, and how I wake up, the Cube, mattress cooling pad keeps me asleep and not waking up in the middle of the night because I'm either too hot or have to use the bathroom.
Question:
What other improvements in your day-to-day routine do you notice since using the Cube?
Answer:
I'm definitely able to focus more and have much more mental clarity. I don't find myself struggling for words or having lots of pauses in my speech, and I definitely have more energy. On days that I work out I'm well beyond where I was before using the Cube and on non-workout days I still have lots of energy to do everything else I need to do!
Question:
What advice would you give friends who might be experiencing sleep struggles associated with common sleep disorders?
Answer:
Turning off your brain, dimming lights, and eliminating distractions that keep your brain awake is a start. If you're waking up tired, having headaches, and feel irritable I would definitely recommend a sleep study. And if you're hot at night, whether you have PTSD, or some other condition that affects your sleep, I can't recommend sleepme enough!
Creating a Safe Space for PTSD Healing and Mental Health Support
Create a safe space. Protect your body and mind. Prioritize a steady sleep schedule and help prevent sleep problems. Then, you can continue working on other self-care habits that will only deepen the relationship with your body and mind that PTSD so often works to destroy.
- National Alliance on Mental Illness (NAMI): (800) 950-NAMI (6264). Available Monday through Friday between 10 a.m. and 6 p.m. EST, hotline staff are prepared to answer any mental health questions you may have. If you prefer, you can also text NAMI to 741741 for free support.
- Substance Abuse and Mental Health Services Administration (SAMHSA): (800) 662-HELP (4357). Available 24/7, 365 days a year, the professionals on the phone can provide treatment information and referrals in English and Spanish to people who have questions about mental health or substance abuse disorders.
- Mentalhealth.gov: (877) 726?4727. This hotline is available between 8 a.m. and 8 p.m. EST to provide mental health information and treatment referrals.
- National Institute of Mental Health (NIMH): 1-866-615-6464(toll-free), 1-301-443-8431 (TTY), or 1-866-415-8051 (TTY toll-free). Available between 8:30 a.m. and 5 p.m. EST, professionals can answer any mental health-related question in English or Spanish and attend to requests for copies of NIMH brochures.