Key Takeaways
PTSD and sleep are deeply connected—addressing sleep disturbances is a critical part of symptom management, recovery, and long-term mental health.
- Sleep disturbances affect the majority of people with PTSD, with insomnia, nightmares, fragmented REM sleep, and night terrors among the most common issues.
- Poor sleep doesn’t just result from PTSD—it can worsen symptoms like anxiety, mood changes, hyperarousal, and difficulty concentrating, creating a self-reinforcing cycle.
- Biological factors such as stress-system dysregulation, altered brain chemistry, and disrupted sleep architecture make restorative sleep harder to achieve in PTSD.
- Effective treatment often combines trauma-focused therapy with sleep-specific approaches like CBT-I, imagery rehearsal therapy, and strong sleep hygiene.
- Improving sleep supports emotional regulation, memory processing, and resilience, making it a foundational component of PTSD recovery.
Post-Traumatic Stress Disorder (PTSD) is a mental health condition triggered by experiencing or witnessing a traumatic event. One of the most significant yet often overlooked aspects of PTSD is its profound impact on sleep.
Individuals with PTSD frequently experience various sleep disturbances, which can exacerbate their symptoms and hinder recovery.
Sleep problems are extremely common in people with PTSD. Up to 80–90% reporting issues, according to a 2023 study by American Psychiatric Association’s journal Psychiatric. [1]
Insomnia symptoms are especially common in PTSD, showing up in about 70–90% of patients, according to a 2018 study published in Behavioral Sleep Medicine that examined insomnia and PTSD symptoms in veterans over time. [2]
Understanding the relationship between PTSD and sleep is vital for effective management and treatment.
Understanding Posttraumatic Stress Disorder
Post-traumatic stress disorder, or PTSD, is a serious mental health condition that can develop after someone experiences or witnesses a traumatic event.
This leaves the brain stuck replaying traumatic memories long after the moment has passed. Think of situations such as combat, natural disasters, or violent attacks. It’s the brain’s alarm system stuck on high alert long after the danger is gone.
According to the DSM-5, PTSD shows up in four main ways. [3] First, there are intrusive memories that crash into your day uninvited. Then there are avoidance behaviors, where you steer clear of anything that reminds you of the event.
It can also shift your mood and thinking in a negative direction. It can intensify your arousal and reactivity. This puts your body in constant tension, jumpy, and ready for danger even when nothing’s happening.
One of the most persistent and disruptive symptoms of stress disorder PTSD is sleep disturbance. This can include trouble falling or staying asleep, frequent nightmares, and restless nights.
These sleep disturbances can seriously affect mental health. They also make it more difficult to recover from trauma, which is why sleep needs to be part of the treatment plan for PTSD.
Take Back Your Night With Chilipad
Better sleep isn’t just helpful when you’re managing PTSD—it’s a lifeline. The Chilipad gives you full control over your sleep temperature, helping calm nighttime restlessness, reduce overheating, and create a better sleep environment your body can depend on.
How PTSD Affects Your Sleep
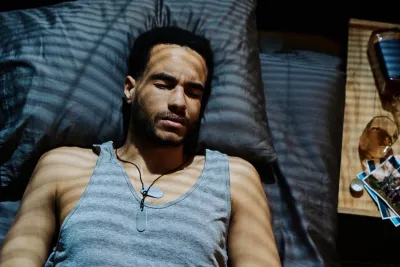
PTSD can easily throw your sleep off track. Many people deal with insomnia, nightmares, night sweats, or even acting out their dreams.
Talking in your sleep, moving around a lot, or having unsettling dreams are all pretty common and can make getting real rest feel tough.
All of these issues fall under the umbrella of sleep disorders linked to trauma. One of them, called Trauma Associated Sleep Disorder, is a specific type of parasomnia often seen in people living with PTSD.
It basically means your brain stays in “danger mode,” even when you’re asleep.
Did You Know: Significant sleep disruptions typically seen in PTSD include fragmented REM sleep and alterations in sleep architecture, such as decreased slow-wave sleep.
Insomnia
A systematic review published in Current Psychology in 2022 found that around 70% of people with PTSD struggle with insomnia. [4]
That means trouble falling asleep, staying asleep, or waking up way earlier than they want to. Because PTSD keeps the body in a hyperalert state, winding down at night becomes difficult, and sleep turns into an ongoing battle instead of something restful.

Nightmares and PTSD
Nightmares are extremely common in PTSD. A review published in Sleep Medicine Reviews found that it affects about 50% to 70% of people. [5]
These dreams are often vivid and tied to a traumatic event, which can cause sudden awakenings and make nighttime feel overwhelming. Over time, this can create a fear of going to sleep, feeding right back into insomnia.
There are treatments that focus specifically on nightmares, like imagery rehearsal therapy as well as medications.
These can help reduce how often nightmares happen and how intense they feel, making sleep a little less intimidating.
Night Terrors and Sleep
During a night terror, someone might suddenly sit up, scream, or look terrified, all while still technically asleep. By morning, they often have no memory of it at all.
These episodes can be distressing for both the person experiencing them and anyone sharing the bed, and they can disrupt sleep in a big way.
Night terrors add another layer of difficulty to already fragile sleep, making restful, restorative sleep even harder to reach.
Nightmares vs. Night Terrors
Night terrors are not the same as nightmares, and the difference matters. Nightmares happen during REM sleep and are usually remembered. Night terrors happen during deep non-REM sleep and are rarely recalled.
Obstructive Sleep Apnea (OSA)
It’s common for people with PTSD to also deal with obstructive sleep apnea, which is a form of sleep-disordered breathing.
A study found a strong link between the two. OSA causes breathing to repeatedly stop and start during the night, breaking up sleep and leaving you exhausted the next day.
Did You Know: Sleep disordered breathing is associated with PTSD and affects 40-90% of patients with the disorder, according to a 2021 review in Sleep Medicine Reviews. [6]
If it isn’t treated, it can make sleep problems worse and intensify PTSD symptoms, creating an even tougher cycle to manage.
Other Sleep Disorders
Sleep can get complicated in PTSD, and several other issues often show up alongside the main symptoms.
This includes dream enactment, unusually light sleep, and Periodic Limb Movement Disorder (PLMD). PLMD, which involves involuntary leg movements during the night, affects about 33% of those living with PTSD. [7]
These disruptions can break up sleep and lead to ongoing sleep loss. It’s also common to see a drop in slow wave sleep — the deep, restorative stage that helps with emotional regulation and memory.
Mechanisms of Sleep Disturbances
The reasons sleep gets disrupted in PTSD, especially among combat veterans, are complex, involving both the mind and the body.
Research shows that the body’s stress response system, especially the HPA axis, often gets thrown off balance. [8] When this system isn’t working smoothly, it can make relaxing and getting steady, restorative sleep much harder.
The HPA axis is the system that controls how your body reacts to stress. When it becomes overactive or out of sync — which is common in PTSD — it can throw off your normal sleep patterns.
This makes it harder for your brain and body to move through the stages of sleep the way they should.
Changes in brain chemistry also play a part. Shifts in neurotransmitters like serotonin and norepinephrine can make it harder to fall asleep, stay asleep, or move through the deep stages of sleep.
These biological changes help explain why insomnia, nightmares, and other sleep disruptions are so common in people with PTSD.

Understanding The Cycle of Sleep Disturbances and PTSD
Sleep problems and PTSD often feed into each other. Sleep issues aren’t just a side effect of PTSD. They’re also considered a core symptom.
PTSD is linked with disrupted REM sleep, including more REM activity and frequent awakenings, which makes restful sleep even harder to get.
Poor sleep can make PTSD symptoms worse. This includes mood changes, irritability, trouble focusing, and daytime hyperarousal or intrusive thoughts. All of this adds up to more daytime fatigue.
On the other hand, those same PTSD symptoms can make it harder to fall asleep or stay asleep, creating a tough cycle that’s hard to break.
The Role of Sleep in Recovery
Sleep is key for emotional regulation and memory processing, including how the brain works through traumatic experiences.
When sleep is disrupted, especially REM sleep. The brain has a harder time organizing and processing those memories.
This can slow down recovery. That’s why treating sleep issues is an important part of managing PTSD symptoms and supporting overall healing.
Assessment of Sleep Disturbances
Accurately assessing sleep disturbances in patients with PTSD is important for developing effective treatment strategies.
Clinicians often use a combination of methods to evaluate sleep problems, including detailed clinical interviews and sleep diaries, where individuals track their sleep patterns and symptoms over time.
For a more comprehensive assessment, polysomnography (PSG) may be used. This overnight sleep study records brain waves, muscle activity, breathing, and other physiological signals to provide a detailed picture of sleep architecture.
They can identify specific sleep disorders, such as sleep apnea or restless leg syndrome.
Additionally, standardized questionnaires like the Pittsburgh Sleep Quality Index (PSQI) and the Insomnia Severity Index (ISI) are valuable tools for measuring subjective sleep quality and the severity of insomnia symptoms.
These assessments help guide treatment decisions and monitor progress over time.
When PTSD Comes with Other Conditions
PTSD often shows up alongside other mental health conditions like depression or anxiety, and this combo can make sleep problems even tougher.
People dealing with multiple conditions may face more intense insomnia, frequent nightmares, and overall more disrupted sleep.
For example, someone managing both PTSD and major depression may have an even harder time falling or staying asleep and may face higher emotional risks.
Anxiety can keep the body on high alert at night, making it difficult to relax enough for good sleep. Because these conditions affect both PTSD symptoms and how well treatment works, it’s important for clinicians to look at the whole picture.
Addressing all mental health factors together can lead to better sleep and better overall outcomes.
How to Sleep Better with PTSD
There are multiple ways people with PTSD can improve their sleep, ranging from lifestyle shifts to targeted therapy and, when appropriate, medication.
Psychological treatments are typically the first line for PTSD-related sleep issues, while medication can be added under professional guidance if needed.
Most treatment plans blend non-drug and drug-based options, tailored to what each person actually responds to.
Working with a sleep specialist can make a big difference, since they can accurately diagnose sleep issues and provide targeted care.
Here are some practical strategies that can help make sleep easier and more restorative for people living with PTSD.
1. Sleep Hygiene
Good sleep hygiene matters more than most people realize. It starts with setting up a quiet, dark and cool bedroom that actually helps your body relax.
Keep the space for sleep and intimacy only so your brain knows what to expect when you walk in.
A steady sleep schedule also helps. For example, going to bed and waking up at the same time every day can train your body to wind down faster and sleep more soundly.
2. Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I is one of the most effective treatments for insomnia and can be especially helpful for people with PTSD.
It teaches better sleep habits, uses relaxation techniques, and helps change unhelpful thoughts around sleep.
One well-known tool in CBT-I is sleep restriction, where you limit the time you spend in bed to match the time you actually sleep. This helps your body rebuild a stronger, more reliable sleep pattern
3. Imagery Rehearsal Therapy
Imagery Rehearsal Therapy helps people take back control of their nightmares. The idea is simple: you rewrite the nightmare while you’re awake, giving it a calmer or safer ending.
Practicing this new version can reduce how often the nightmare shows up and how intense it feels. It’s especially useful when the dreams are tied to the trauma itself.
4. Healthy Lifestyle Choices
Simple daily habits can make a big difference in sleep. Regular movement, a balanced diet, and avoiding caffeine or heavy meals before bed can all help your body settle for better sleep.
Everyone’s different, so it’s worth trying a few of these habits to see which ones actually help you sleep better while managing posttraumatic stress disorder.
5. Relaxation Techniques
Wind-down routines can make a big difference for sleep, especially if you’re dealing with posttraumatic stress disorder. Simple calming activities before bed can help lower anxiety and ease your body into rest.
This might look like reading a light book, taking a warm bath, stretching, listening to calming music, soothing sounds, or trying a guided meditation.
You can mix and match to see what helps you feel the most relaxed.
Give a few of these a try to see which ones work best for you. It can take some time to figure out your ideal routine, so be patient with yourself.
Help is Available: When to Seek Help
If post-traumatic stress disorder symptoms last more than a month or start getting in the way of daily life, it’s time to reach out for support.
This includes things like reliving the event, avoiding reminders, feeling constantly on edge, or dealing with mood changes.
A healthcare professional can help sort through your symptoms and offer strategies that fit your situation, including support for sleep problems.
If you need immediate help or someone to talk to, you can contact:
- 988 Suicide & Crisis Lifeline — Call or text 988
- SAMHSA National Helpline — 1-800-662-HELP (4357)
- National Center for PTSD — visit their website
You don’t have to manage this alone. Reaching out is a strong first step.
Final Thoughts
PTSD and poor sleep feed off each other, creating a loop that can feel impossible to break. Treating PTSD itself—through options like EMDR, trauma-focused CBT, prolonged exposure, or medication support—helps lower daytime stress and makes nighttime recovery easier. Pairing those therapies with sleep-focused tools like CBT-I, imagery rehearsal therapy, and steady sleep habits gives your brain a better shot at shutting down the “alert mode” that keeps you up. Good sleep won’t erase trauma, but it strengthens the stability, clarity, and resilience you need to move forward. With the right mix of PTSD treatment, smart sleep strategies, and support from a specialist, calmer nights—and brighter days—are absolutely within reach.
Frequently Asked Questions About Sleep and PTSD
How do sleep issues affect PTSD symptoms?
Sleep problems like insomnia and nightmares are common in PTSD and can worsen symptoms. They interfere with memory processing and emotional regulation, slowing recovery.
What are the common sleep problems associated with PTSD?
- Insomnia: Affects about 90% of those with PTSD due to hyperarousal and stress.
- Nightmares: Vivid dreams related to trauma disrupt sleep.
- Obstructive Sleep Apnea (OSA): More common in PTSD patients, possibly linked to chronic arousal.
How does PTSD affect sleep?
People with PTSD often struggle to fall asleep, wake frequently, and experience non-refreshing sleep. Conditions like chronic pain or depression can worsen sleep quality.
How canI improve their sleep?
- Maintain a cool, dark, quiet environment.
- Stick to a regular schedule.
- Avoid caffeine and heavy meals before bed.
- Exercise regularly.
- Practice relaxation techniques.
How can family members support someone with PTSD and sleep issues?
Family members can help by creating a supportive environment, encouraging healthy sleep habits, and being understanding of the challenges faced by their loved one.
Peer-Reviewed Research References
-
So, C. J., Miller, K. E., & Gehrman, P. R.
Sleep Disturbances Associated With Posttraumatic Stress Disorder.
Psychiatric Annals, 53(11), 491–495, 2023.
Source Type: Peer-Reviewed Clinical Review
Key Insight: Reviews the wide range of sleep disturbances linked to PTSD, including insomnia, nightmares, fragmented sleep, and hyperarousal, emphasizing sleep as a core component of PTSD symptom severity.
View Study
-
Colvonen, P. J., Ellison, J., Haller, M., & Norman, S. B.
Examining Insomnia and PTSD Over Time in Veterans in Residential Treatment for Substance Use Disorders and PTSD.
Behavioral Sleep Medicine, 17(4), 524–535, 2019.
Source Type: Longitudinal Clinical Study
Key Insight: Demonstrates a bidirectional relationship between insomnia and PTSD symptoms over time, showing that persistent sleep disturbance predicts poorer treatment outcomes in veterans.
View Study
-
BMJ Best Practice.
Post-Traumatic Stress Disorder: Symptoms, Diagnosis, and Treatment.
Source Type: Clinical Practice Guidance
Key Insight: Provides evidence-based clinical guidance on PTSD diagnosis and management, identifying sleep disturbance and nightmares as central diagnostic and treatment targets.
View Resource
-
Isaac, F., Toukhsati, S. R., DiBenedetto, M., & Kennedy, G. A.
Cognitive Behavioral Therapy-Based Treatments for Insomnia and Nightmares in Adults with Trauma Symptoms: A Systematic Review.
Current Psychology, 2022.
Source Type: Systematic Review
Key Insight: Finds strong evidence supporting CBT-I and imagery rehearsal therapy (IRT) for improving insomnia and trauma-related nightmares in adults with PTSD symptoms.
View Study
-
Hasler, B., & Germain, A.
Correlates and Treatments of Nightmares in Adults.
Sleep Medicine Clinics, 4(4), 507–517, 2009.
Source Type: Clinical Review
Key Insight: Explores physiological and psychological contributors to chronic nightmares and reviews pharmacologic and behavioral treatment approaches, particularly in trauma-exposed populations.
View Study
-
Lancel, M., van Marle, H. J. F., van Veen, M. M., & van Schagen, A. M.
Disturbed Sleep in PTSD: Thinking Beyond Nightmares.
Frontiers in Psychiatry, 12, 767760, 2021.
Source Type: Peer-Reviewed Review Article
Key Insight: Argues that PTSD-related sleep disturbance extends beyond nightmares to include REM fragmentation, altered sleep architecture, and autonomic dysregulation.
View Study
-
Cleveland Clinic.
Periodic Limb Movements of Sleep (PLMS).
June 8, 2023.
Source Type: Medical Reference Resource
Key Insight: Explains periodic limb movements during sleep, which are more prevalent in individuals with PTSD and can further fragment sleep and worsen insomnia symptoms.
View Resource
-
P. S., & Vellapandian, C.
Hypothalamic-Pituitary-Adrenal (HPA) Axis: Unveiling the Potential Mechanisms Involved in Stress-Induced Alzheimer’s Disease and Depression.
Cureus, 16(8), e67595, 2024.
Source Type: Mechanistic Review
Key Insight: Reviews how chronic stress dysregulates the HPA axis, contributing to sleep disruption, mood disorders, and long-term neurodegenerative risk.
View Study









